
The government has recently launched a new vaccine program for young girls aged between nine and thirteen years old. However, there has been a wave of disagreement and hesitation concerning the vaccination. This week we met a gynaecologist and Link to Life Coordinator to highlight the importance of HPV vaccine and shed more light on cervical cancer.
Publicité
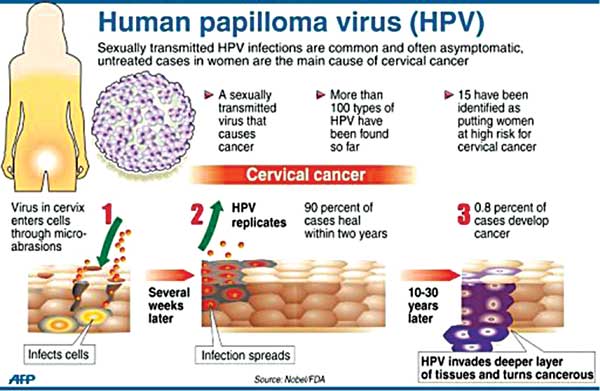
Human papillomavirus (HPV) has long haunted humankind. Almost all sexually active adults carry some of HPV’s 170 strains. After years of tireless efforts, scientists came up with a vaccine known as HPV. It is an important vaccine as it protects the human body against cancers caused by HPV infection. The World Health Organisation has initiated a Global Vaccine Action Plan (GVAP) signed by 194 states in 2012. It is a framework to prevent millions of deaths by 2020 through more equitable access to existing vaccines for people in all communities.

Dr Shilpa Sinha, Obstetrics and Gynaecologist at Apollo Bramwell Hospital, explains that HPV vaccine is safe and effective vaccine protects people from most of the cancer caused by human papillomavirus infection. “HPV is the most common sexually transmitted infection. More than 100 varieties of Human papillomavirus exist but around 40 HPV types can infect the genital areas of males and females. They can also infect the mouth and throat. Most people with HPV never develop symptoms or health problems. Most HPV infection (9 out of 10) go away by themselves within two years. But sometimes HPV infection will exist and can cause cancer of cervix, vagina and vulva in women, cancer of penis in men or cancer of anus or back of throat including base of tongue and throat (oropharynx) in women and men and cause genital warts in men and women,” she reveals.
Link to Life Coordinator Selvina Moonesawmy points out that for the age of 11-14, two dosages are given while as from the age of 15 onward, three dosages are given. “For the vaccination to work more efficiently, it should be given to young girls. The vaccination should be done before any girl is sexually active.”
Importance of the vaccines
Selvina Moonesawmy explains that since 2013, Link to Life had already started the vaccination programme with 300 young girls from vulnerable areas. “We went in different poor region around the Island so that young girls are vaccinated. Before implementing this programme, a session was carried out with parents so that they are better informed about the vaccination,” she adds.
Highlighting the importance of the vaccination, Selvina avers that the vaccination ensures the protection of young girls against HPV by 70%. “The vaccination helps build antibodies to destroy various viruses that the body cannot eliminate on its own. There are certain types of virus that the body can eliminate on its own. So it is important to protect our young girls from other viruses too.”
Similarly Dr Shilpa Sinha states that girls should receive all doses of HPV vaccine long before they begin any type of sexual activity and are exposed to HPV. “HPV vaccine produces a higher immune response in preteens than it does in older teens and young women. Even if someone has already had sex they should still get HPV vaccine. You may have one strain of HP virus; the vaccine can protect you from other strains that you haven’t been exposed yet,” she explains.
Statistics
As far as the statistics are concerned, 150 new cases are detected every year and 50 death cases are registered annually in Mauritius. For the last 12 years, the average years of women affected are 56 years. However, the rate of cervical cancer is in decreasing trend. It is now ranked third in death causing cancer.
Side effects
Vaccines like any other medications may have side effects. Many people who get HPV vaccine have no side effects at all. As advanced by Dr Sinha, some of the main symptoms include the following:
- pain, redness or swelling in the arm where shot was given
- fever
- nausea
- headache/fatigue
- muscle or joint pain
- sometimes dizziness or fainting spells (remaining sitting or lying for 15 minutes after vaccination helps preventing this)
- rare severe (anaphylactic) allergic reaction can occur if allergic to any component of vaccine.
Selvina Moonesawmy, on her part, advocates that she did not see any major side effect in 300 young girls vaccinated. “The vaccination has been tested and is used worldwide. There are no major side effects. Patients can get minor effects like headache or psychological misbalance because of stress. However, before the vaccination, it is important to have a medical history of the patient. There are certain information that is needed like sexual activity, pregnancy or serious health issues. In case of pregnancy, the vaccination cannot be done.”
Why so much hesitation?
One main question is why people are hesitant for the vaccination. Dr Shilpa Sinha states that safety concerns about HPV vaccine and worries about the side effects prevent some parents from giving the vaccine. “Some parents believe that this vaccine is not needed. Some parents put off the HPV shots because their daughters are not sexually active- a mistaken justification because doctors recommend giving the vaccine at age of 11 or 12 years before a teen becomes sexually active. Some parents are afraid that giving vaccine acts as a sort of permission for teens to be sexually active.”

How do HPV vaccines work?
Like other immunizations that guard against viral infections, HPV vaccines stimulate the body to produce antibodies that, in future encounters with HPV, bind to the virus and prevent it from infecting cells. The current HPV vaccines are based on virus-like particles (VLPs) that are formed by HPV surface components. VLPs are not infectious, because they lack the virus’s DNA. However, they closely resemble the natural virus, and antibodies against the VLPs also have activity against the natural virus. The VLPs have been found to be strongly immunogenic, which means that they induce high levels of antibody production by the body. This makes the vaccines highly effective. The VLP technology that is used in the HPV vaccines was developed by NCI and other scientists. NCI licensed the technology to Merck and GSK to develop HPV vaccines for widespread distribution.
Smear test
Another means of prevention is Smear or Pap test. A smear test (sometimes called a pap test) is used for cervical screening. It is a simple procedure where a doctor or nurse takes a sample of cells from the cervix (neck of the womb) to be examined for early changes on the cells. “Smear test is just a normal test to determine the health status of the uterus. It helps to diagnose any infection or inflammation in the uterus. It is crucial that every woman does it,” Selvina explains.
According to the coordinator, every two years, a woman who is sexually active should undergo a smear test. “One year after a woman has had her first sexual intercourse, she should examine herself. It is a means for prevention. It is necessary to go for a diagnosis before the symptoms of cervical cancer start to appear. If anomalies are detected beforehand, it becomes easier to tackle the health issue.”
HPV Vaccine: Myth versus Facts
MYTH: The vaccine has caused many deaths.
FACT: No causal link between the vaccine and death has been found. The safety of Gardasil vaccine has been carefully evaluated since 2002. It is in wide use internationally with over 120 million doses administered.
MYTH: The clinical trials did not prove that the vaccine prevented death from cervical cancer.
FACT: The trials could not ethically allow cervical cancer or death to be end points for evaluation. Women who developed cervical abnormalities were treated to prevent cancer. The trials show almost 100% efficacy in the prevention of high grade HPV types 16 and 18 related pre-cancers, which cause 70% of cervical cancers.
MYTH: The vaccine can make pre-existing HPV infections worse.
FACT: Clinical studies show no worsening of pre-existing diseases. The vaccine does not treat an existing HPV infection and ideally should be given prior to being sexually active.
MYTH: The vaccine only lasts 5 years
FACT: Current data suggests the vaccine protection is ongoing, with no sign of waning. The mechanism of immune memory has been demonstrated in women who have been vaccinated, indicating the vaccine will provide long-term immunity.
MYTH: The vaccine affects fertility and if given to young girls might make them infertile.
FACT: Gardasil does not cause infertility or sterility.
MYTH: The vaccine can cause birth defects.
FACT: No specific congenital abnormalities resulting from the vaccine have been demonstrated. In the clinical trials, the pregnancy rates and congenital abnormalities were the same in both vaccinated and placebo (non vaccine) groups.
MYTH: Because the clinical trials of the vaccine didn’t include girls under 16, the vaccine is not proven to be safe for girls less than 16 years
FACT: The clinical trials included girls aged from 9 years of age, who were tested for their immune response to the vaccine and followed up for safety. It would have been unethical to have subjected these girls to cervical smears at this younger age. The group who received the vaccine in early adolescence has now been followed as young adults, with no development of the HPV infections covered by the vaccine.
MYTH: The vaccine has caused many serious adverse reactions.
FACT: Gardasil has not been found to cause increased risk for any serious condition.

Notre service WhatsApp. Vous êtes témoins d`un événement d`actualité ou d`une scène insolite? Envoyez-nous vos photos ou vidéos sur le 5 259 82 00 !















![[Info Soirée] : L'ex-Commissaire de Police, Anil Kumar Dip, fait l'objet d'une nouvelle plainte](https://defimedia.info/sites/default/files/styles/square_thumbnail/public/thumbnail_181224.jpg?itok=VJgXLMjW)





